Physical Therapy for Postpartum Urinary Stress Incontinence
Postpartum urinary stress incontinence occurs when an individual experiences involuntary urine leakage that happens during activities like coughing, sneezing, laughing, squatting, or impact movements following pregnancy and childbirth, often due to pelvic floor dysfunction. Approximately 34% of women experience urinary incontinence postpartum. Physical therapy has been shown to be 80% effective at treating urinary stress incontinence. Pelvic floor physical therapy is used to treat urinary incontinence, a program of functional retraining to improve pelvic floor muscle strength, endurance, power, and relaxation. Mangiarelli Rehabilitation physical therapist Jen demonstrates three exercises you can do for urinary stress incontinence in the video below!
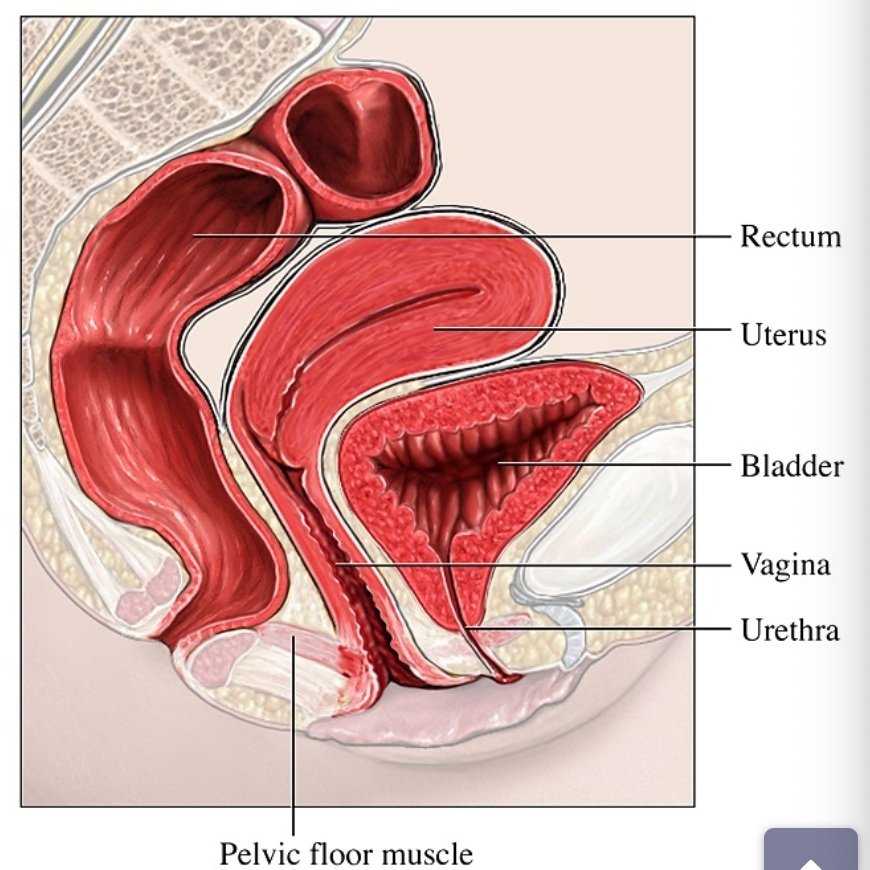
Pelvic Floor & Bladder Anatomy
The pelvic floor is located between the tailbone and the pubic bone within the pelvis, composed of striated muscles arranged in a dome-shaped sling. The pelvic floor muscles lift and support internal organs like the bladder and uterus, form the foundation of the core muscles, support the low back, stabilize the pelvic bone, help with sexual function, and control the sphincter muscles, ringlike muscles that open and close certain body openings like the urethra.
The continence mechanism of the bladder is embedded within the pelvic floor structure. The pelvic floor muscles surround the urethra, the tube through which urine leaves the body, helping to keep it closed when pressure is placed on the bladder. Pelvic floor muscle contraction can increase the urethral pressure and elevate the urethra under the pubic symphysis (joint between left and right pelvic bone) to maintain continence and prevent urinary leakage.
What is Postpartum Urinary Stress Incontinence?
Urinary stress incontinence occurs when an individual experiences involuntary urine leakage that happens during activities like coughing, sneezing, laughing, squatting, or impact movements. Stress incontinence can develop after pregnancy and childbirth due to the effect of pregnancy and childbirth on a woman’s pelvic floor. During pregnancy, hormonal changes increase the laxity of the pelvic floor muscles and the weight of the growing uterus and baby places increased pressure on the pelvic floor. During childbirth, especially vaginal delivery, pelvic floor muscles can weaken and even tear, which can dramatically affect bladder control and continence after birth.
Approximately 34% of women experience urinary incontinence postpartum. Women are more likely to develop urinary stress incontinence if they have bladder issues during pregnancy or have had bowel or bladder problems prior to pregnancy, if this is their first baby or a very large baby, if they have a long labor, or if they have a difficult delivery, requiring stitches for tearing or the use of forceps or a vacuum cup during delivery. Vaginal delivery increases the risk of developing postpartum stress incontinence (40.3%); 28.8% for women who deliver via c-section develop postpartum urinary incontinence. However, having three or more cesarean deliveries can make it just as likely to develop bladder issues as those who give birth vaginally.
Physical Therapy Treatment for Urinary Stress Incontinence
Physical therapy has been shown to be 80% effective at treating urinary stress incontinence. Pelvic floor physical therapy is used to treat urinary incontinence, a program of functional retraining to improve pelvic floor muscle strength, endurance, power, and relaxation in women with pelvic floor dysfunction. Our therapists combine pelvic floor rehabilitation with manual therapy, electrical stimulation, bladder retraining, and lifestyle education.
The physical therapist first completes a thorough evaluation, assessing the pelvic and abdominal area and lumbosacral and SI joints and evaluating the tone, elasticity, strength, and areas of tenderness and pain of the pelvic floor muscles through an internal exam (with consent of the patient). The therapist will also review the patient’s bladder habits and lifestyle factors that could be contributing to urinary incontinence as well as discuss the delivery and its affect the pelvic floor. From there, the therapist designs a targeted treatment program customized to the patient’s condition and goals.
Mangiarelli Rehabilitation physical therapist Jen demonstrates three exercises you can do for urinary stress incontinence in the video below. Jen outlines the importance of starting with gentle walking to engage your pelvic girdle and then progressing to band and ball exercises to work your outer and inner thigh muscles to begin to move the body and initiate gentle engagement of the pelvic floor muscles.
When a woman is ready to start physical therapy to strengthen and heal the pelvic floor and address urinary incontinence, treatment can include:
Manual therapy: involves internal stretching of specific pelvic floor muscles as well as soft tissue mobilizations around scar tissue and connective tissue restrictions in the abdomen, pelvis, and inner thighs. This not only relieves tightness in these areas, but also improves blood flow to the tissues, muscles, and nerves to promote healing.
Electrical stimulation: The therapist may use electrical stimulation to help the patient contract the pelvic floor and assist the patient in isolating the proper pelvic floor muscles for strengthening using a gentle electric current on the specific muscle.
Bladder retraining: self-regulation of bladder continence, gradually retraining the bladder so that visits to the bathroom extend to 2.5 to 3 hours between visits.
Strengthening exercises: using kegel exercises to repeatedly tighten and release the pelvic floor muscles to build coordination and endurance through contracting and quickly relaxing the muscles, enhancing the muscles’ holding ability.
Therapeutic exercise: specific strengthening of the hip, pelvic, and core muscles to provide additional support for proper bladder function.
Patient education: education on lifestyle factors, like reducing caffeine intake and limiting spicy or citrus foods that can irritate the bladder as well as relaxation techniques of the bladder and pelvic floor muscles.
Numerous studies have shown that pelvic floor physical therapy is effective in addressing postpartum urinary stress incontinence. In a 2018 meta-analysis of 15 randomized control trials assessing the effect of postpartum pelvic floor physical therapy (PFPT) on pelvic organ prolapse, sexual function, and incontinence found that women who received PFPT were less likely to report urinary incontinence up to 12 months postpartum.
A 2020 study evaluated the effect of individualized physical therapy-guided pelvic floor muscle training in the early postpartum period on urinary incontinence and pelvic floor muscle strength and endurance. Eighty-four participants who were 6-10 weeks post-delivery and were experiencing urinary incontinence took part in the study. Forty-one women were in the intervention group which involved 12 weekly sessions with a physical therapist for pelvic floor training, while 43 women were in the control group who were given no instructions after their initial assessment. Researchers found that urinary incontinence was less frequent in the intervention group (21 intervention participants still had symptoms vs. 31 of the control group) after treatment and that the intervention group had improved pelvic floor muscle strength and endurance at 12 months post-intervention.
Another study evaluated 52 women with persistent stress urinary incontinence three months after delivery with two different interventions. The first group had 8 weekly physical therapy sessions that involved electrical stimulation of the pelvic floor muscles followed by pelvic floor exercises with biofeedback and a home exercise program. The second group received the same intervention as well as additional deep abdominal muscle training. The control group received weekly massages of the back and extremities and did not complete pelvic floor exercises. The researchers found that urinary leakage did not occur in 56% of the first group and 74% of the second group, but all women in the control group continued to have urinary leakage. The eight weeks of pelvic floor therapy was effective in curing 70% of the women who received the physical therapy intervention.
Postpartum urinary stress incontinence can be debilitating and embarrassing. Work with a physical therapist today to address your urinary incontinence and get back to the activities you love!